Cervical Region (neck)
Likely the second most common area you will treat in your entire career. The cervical region can in of itself be the main driver of pain or it can be linked to the shoulder, jaw, thoracic and entire upper limb depending on the condition.
Starting with a general overview of anatomy then we will cover the most common type of conditions you will see in the clinic. Followed by how to assess and the concepts behind treating those conditions.


Structural Overview
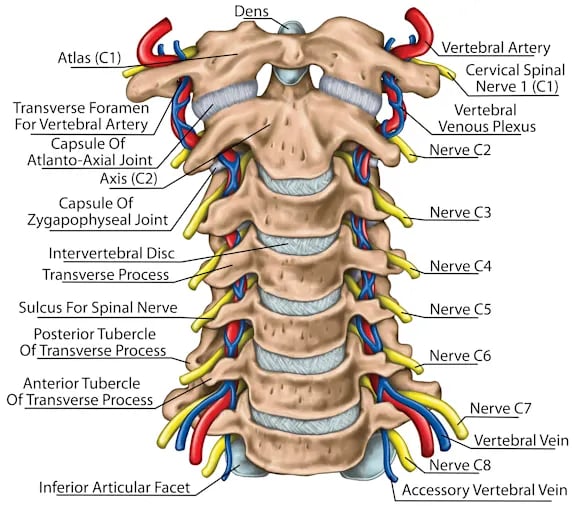
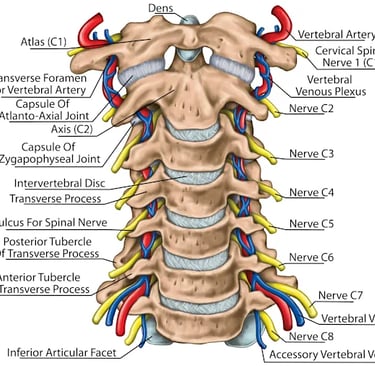
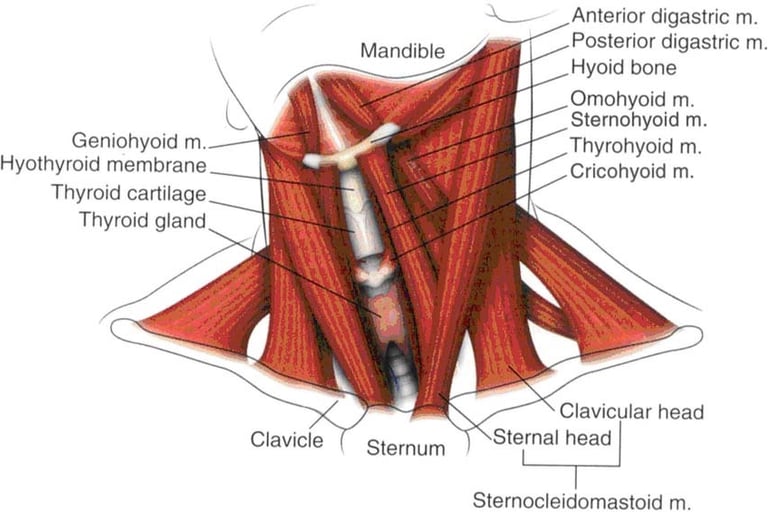
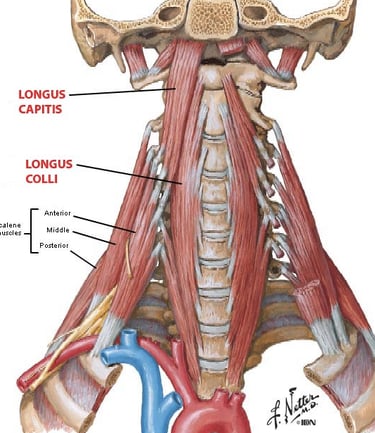
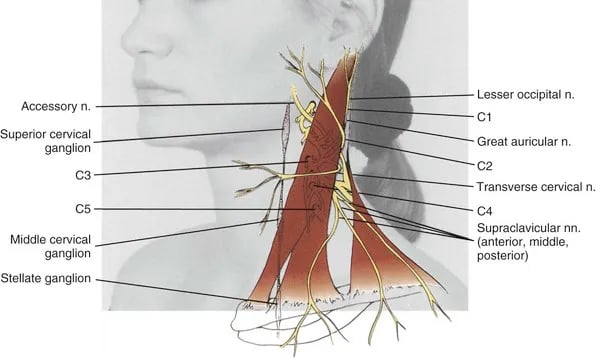
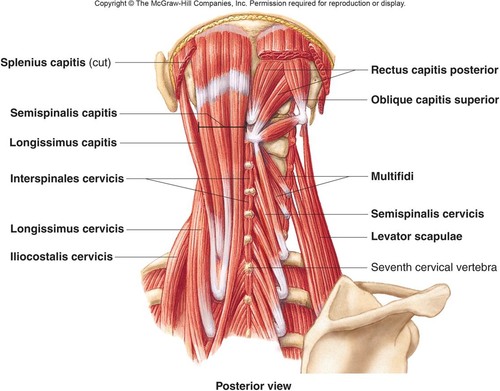
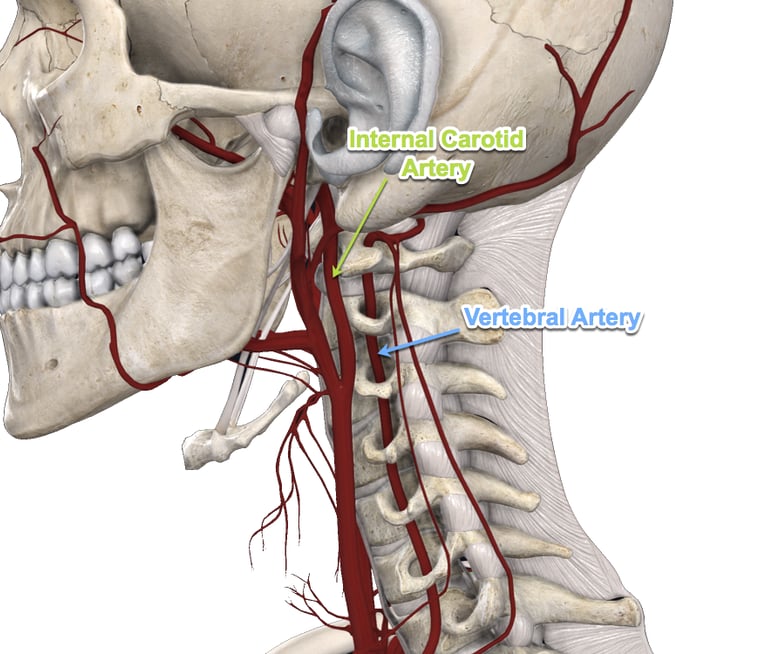
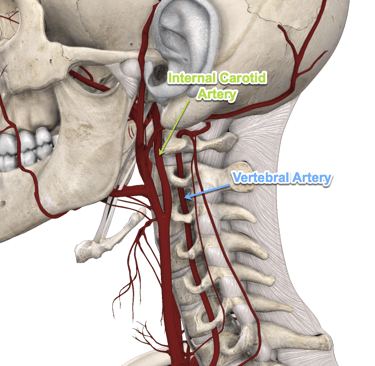
7 vertebra and the associated myotomes/dermatomes, Brachial Plexus, first rib, C2, circle of willis, are but a few of the structures around the neck that play a role in our patients pain and dysfunction. You can always come back to this page to review your anatomy of all levels but the better your palpation becomes and mobilisation skills the better your understanding of how the anatomy actual plays its part.
Common Conditions
Wry Neck: Super common, very benign but can be very stressful for the patient. Make sure the clear of anything serious and if so educate the patient to decrease the anxiety and stress level, make sure not the underplay it either. Usually caused by a mixture of stress, different pillow/bed, extreme neck ranges in sports and in some presentations the patient is unable to divulge anything that could be a cause. Patient often present with a very rigid neck posture globally and/or limited range in one specific direction. Basic Treatment: soft tissue release, G1 mobs, education, heat, NWB ROM
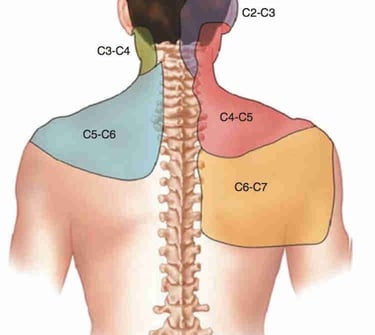
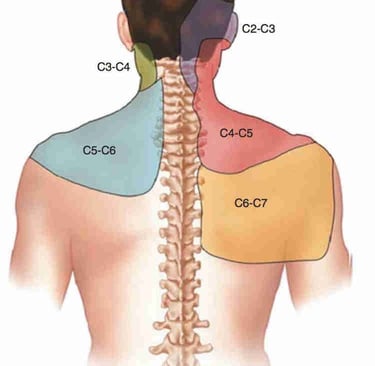
Cervical Radiculopathy: Pure nerve root pain caused by disc herniation or bone changes. Occurs more in the 40s plus patient range. Can be insidious or triggered by a trauma. Patients will often have radiating pain from the neck into the shoulder and often the entire upper limb in a dermatomal pattern. It can be pain, pins/needles, numbness, weakness and headaches can occur also. True positive is positive on ULTT, spurlings (if already sure skip as this will greatly aggravate symptoms) and distraction. Patients are often more comfortable being treated in sitting and will often sleep in a recliner or a propped up position. Basic Treatment: Education (starts to improve around 6/52 mark, TPDN, auxiliary sling, nerve glides.
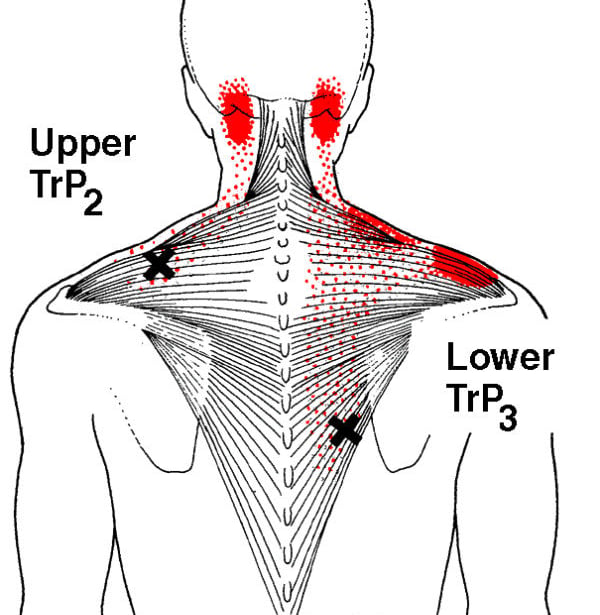
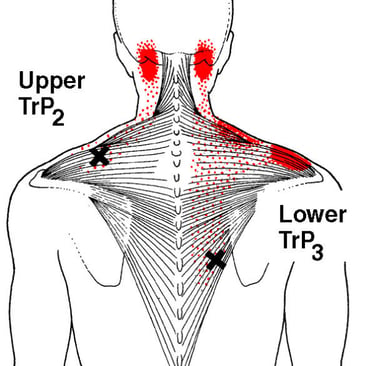
Facet joint Overload/Aggravation: As it sounds pain driven by the facet joints. Typically due to repetitive actions and in the older population but can be seen in contact sports also. Pain with often be unilateral and movements that cause pain will primarily be rotation away and lateral flexion towards. Pain typically follows the image to the right. Basic Treatment: STR, GENTLE mobs to opposite side and above/below aggravated side. Education on avoiding provocative positions/ activities. Keep DNF engaged and pain free ROM working. Long term build general neck strength and SLOWLY return to aggravating activities IF required (eg. sports).
Disc bulge: For many the worst news a patient can hear and a sign that they now have a 'bad' neck. This is simply not the case. Painful yes, but many patients with the right approach and attitude can make excellent if not full recoveries. Although the main mechanism is forced flexion with rotation patients have reported a multitude of mechanisms that have triggered symptoms. The key is to educate to ensure the patient has a more positive attitude relating to the type of injury which the research and anecdotal evidence shows has far better outcomes. Patients report pain, burning, numbness, pins/needles, weakness and stiffness. The symptoms can be central or unilateral and can follow a dermatomal pattern or nerve pathway pattern. Basic Treatment: symptom relief proximal and distal, gentle STR, TPDN, NWB ROM exercises, Mckenzie based exercise (positions of relief). scans are generally not recommended unless nil progress is being made after the first few weeks. Although the bulge can never strengthen it will stabilise and callous up. Timeframes can be risky as patient can become very anxious should pain or symptoms move pats this time frame. Generally 2 to 8 weeks, some can be much fast while others can sensitise and become chronic.
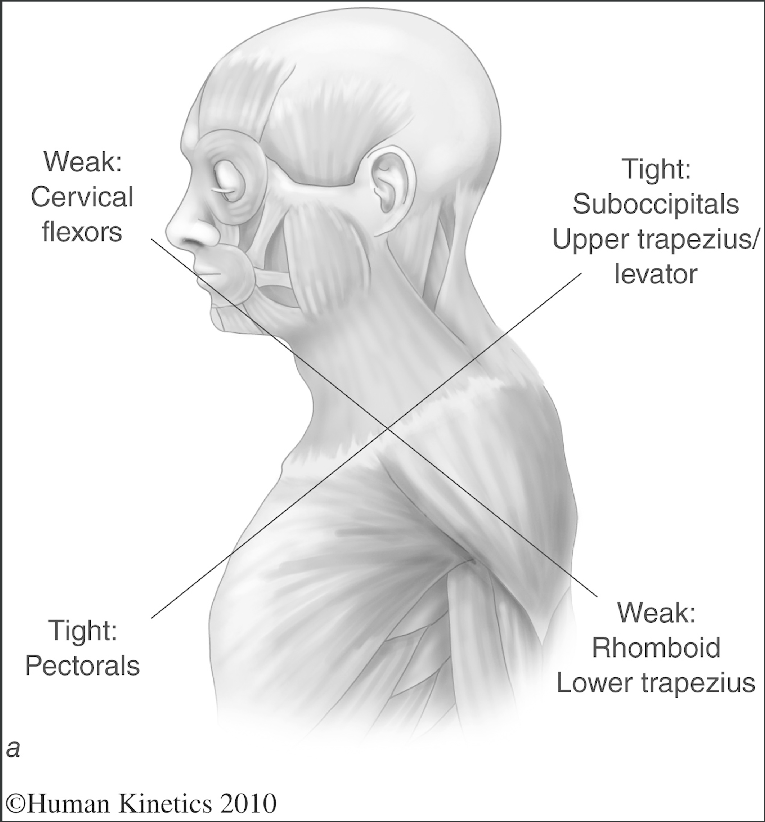
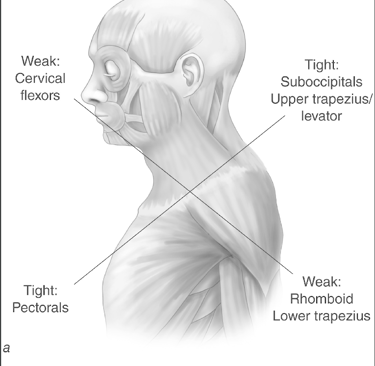
Upper Cross Syndrome: A less used term than previous years. This describes the classic presentation of Tight: pecs/traps and Weak: SCM/low traps. Patient posture will often be very rounded common complaints include neck and/or mid back pain or stiffness, head aches, eye strain, shoulder pain when lifting overhead. . This can also contribute to TMJ related issues also. These patient benefit greatly especially early on from self release with a trigger ball, strength can be effective but use sparingly. Basic Treatment: release tight areas and strengthen weak areas. Later on strengthen tight areas through range. Educate on posture and breaks time for sitting/computer.
Postural Overload: A more focused version of upper cross syndrome to one, sometimes two areas. This general affects the neck. Poke neck or text neck is another term. Patients with high stress positions and or excessive screen time. Patients often reports headaches, base of skull pain, tempolar tension and very tight traps. A similar approach as upper cross syndrome can be used with an emphasis on education around posture. Do not be afraid to talk about proper tongue posture and breathing patterns as the thousands of reps we do per day have a huge accumulative effect. Basic Treatment: teach postural awareness with taping, strengthen the upper back and educate+++.
C2 headache: Exactly as it sounds a dull head ache that is purely brought on by the C2 vertebrae being misaligned. The pain can be reported as behind the eye or in a headband type pattern. On palpation in supine often the C2 vertebra will be sitting towards one side more that the other OR will no rotate as the head is rotated passively in full neck flexion. Basic Treatment: STR and mobs of C2 to centre as a start
Whiplash Associated Disorder: Patient will often present while being covered by CTP insurance. Presentation can vary greatly as will progression. The below grading sheet is helpful as a general rule.
Patients can have headaches, fear of movement, radiating pain, dizziness, greatly increased neck muscle tone, disrupted sleep patterns and very very tender on palpation. Basic treatment: decrease tone and fear of movement then rebuild neck strength and endurance starting with DNF training. This slowly turns into a general exercise program with an emphasis on neck and shoulder training.
Shoulder Related Neck pain: as you have seen from the section on facet joint pain the neck can refer pain to the shoulder. It can also work in reverse but in a more general sense (dysfunctional shoulder looking to the neck to help stabilise and perform functional tasks). It can also be very specific in relation to trigger point referral patterns. For example the low trap, levator scap and lateral upper trap can all refer pain to the base of the neck. Basic Treatment: be very thorough in assessment, clean the shoulder and feel the muscle tone left vs right around the shoulder if you suspect it could be a potential driver.
Subjective Concepts
As best practice it is recommended to get into the habit of clearing VBI (5Ds, 3Ns). This not only ensures you are likely to never miss an occurrence but also show the patient that anything truly concerning is not present in their condition.
5 Ds: diplopia, dizziness, drop attacks, dysarthria, dysphagia
3 Ds: nausea, numbness, and nystagmus
Main points to hit with anything neck related should include:
-insidious vs traumatic
-Acute vs chronic
-LOC if any
-Timeframe
-Referral pattern if any
-NPS (you will get a feel for when patients do not fully understand this. Some patients have naturally two scores, one for ache like pain and one for actual pain)
-Painful movements
-Heat vs ice effect
-Yellow flags (anything spinal can be heavily influenced by a persons level of anxiety or current level of mental health, positive and negative)
The above are a general rules but make sure the follow your patient in the subjective if you believe it will lead to relevant information about long term treatment.
Objective Assessment
The below is general order but should be modified as needed to suit the patients current state.
VBI if indicated
Static posture (look at alignment through all planes, poke neck, trap position)
AROM Cx (F/E/LF/ROT, quadrant only if late stage rehab or looking for more answers)
AROM Tx (F/E/ROT/LF, if the thoracic is limited the cervical will often try to pick up the slack)
Clear shoulder (AROM shoulder, CUFF strength and to see how involved TRAPS/SCM in arm actions)
Palpation (sitting or supine)
-C1 region
-LATERAL movement along each side of Cx for pain/stiffness
-1st ribs
-TRAP and SCM tension
PROM in supine
ALWAYS re-test, ALWAYS.
This can either be at the end of the session or immediately after the first section of treatment if you are unsure of the effect and if you time is better spent elsewhere.
If there is a change in symtpoms/movement this can be incredibly motivating for the patient and should not be overlooked.
It also obviously shows you if you're on the right path.
Treatment Strategies and Concepts
Even though some of the best treatment are provided in the common presentations here is a cheat sheet of what to do for what problem.
Once again, general rules and use it as it fits into the clinical picture.
High muscle tension: STR/ART/DTR, TPDN, Self release techniques, gentle passive stretches
Joint Stiffness: mobs, G2/3/4
Joint pain: Mobs G1/STR, heatpack, TPDN, traction
Joint Instability: strength work starting with isometrics and general in a supported positions
Movement Dysfunction: general idea is trying to get closer to balance. how do you turn down the volume
on the structures doing too much and how to get the underachieve areas move involved.
Fear of movement: education, reassurance, NWB PROM exercises