Shoulder Girdle


Many physiotherapist fear the shoulder. They think it is too complex or that the assessment isn't as accurate as it should be or if the 4 pack doesn't work then all is lost.
The truth is the shoulder CAN be complex and it CAN take time to progress especially if overload based. The key is to look for common patterns in subjective and objective, then look for the cause. As except for a traumatic injury the 'site of pain is not the source' could not be more true than at the shoulder.
Go in with a good attitude. Then every shoulder is a chance to learn more clinical patterns, refine your assessment techniques and be able to deduce more key info from the subjective. In time the shoulder will be no more a mystery than any other joint.
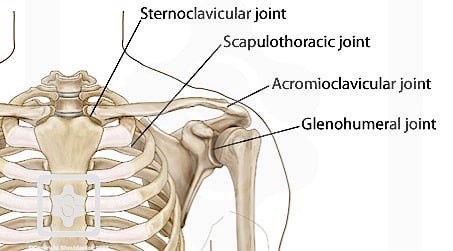
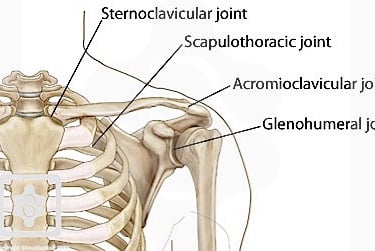
4 Joints per side, Not 1
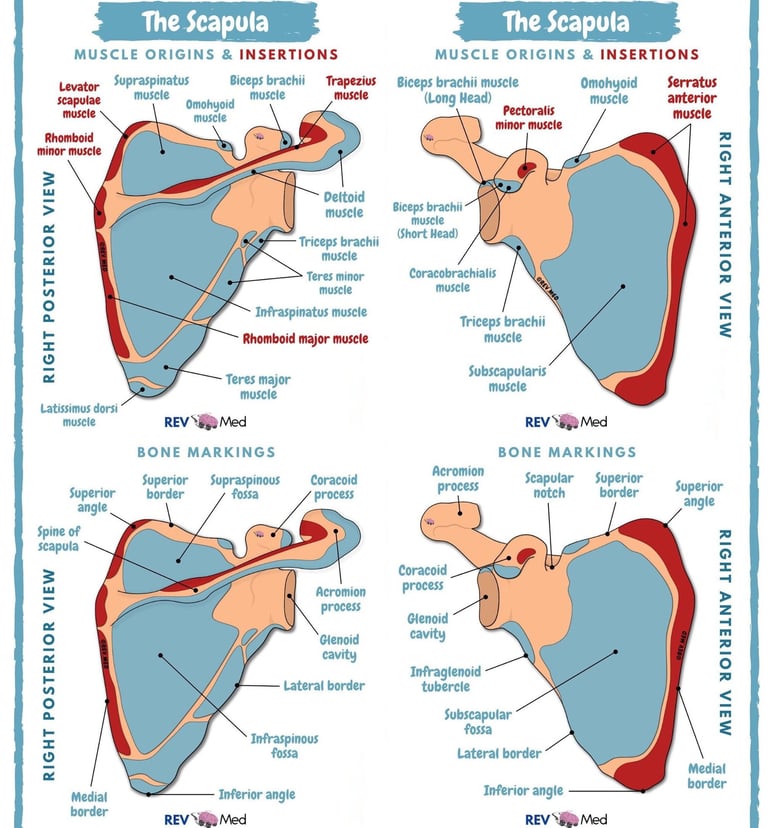
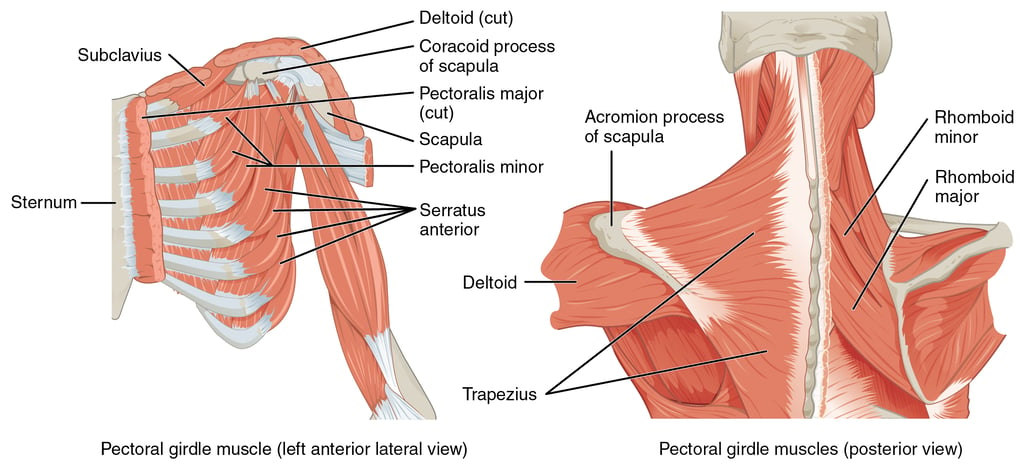
As with every section lets begin with the structural overview so you can better understand the interplay at the shoulder girdle. As a note please do not try to memorise every single structure but use this page to come back to again and again to ensure you can visualise what is going on beneath the surface.
Acromioclavicular Joint: Involved with many more overhead/abducted arm. positions. When this area is aggravated any compressive/distraction based force (ER/IR) movements can be painful. Old ACJt injuries can make this area look very pronounced but are often still funny functional.
Glenohumeral Joint: What most of us think about when we say shoulder. The amount of actual bony contact for the head of humerus and glenoid is about the size of your thumb print. Making not just the CUFF but also the muscles that surround the shoulder very important in stability. Mobility comes at the cost of stability and is a huge reason why this area is so often injured.
Sternoclavicular Joint: Under appreciated in the role it plays. Every movement at scapulothoracic joint affects this area. Subtle yes but still important and can be a driver of pain down stream if hyper/hypomobile. When you retract the scaps the SCJt glides forward, when you raise your arm overhead it depresses. The reverse is also true.
Scapulothoracic Joint: Technically not a true joint but without it our shoulder stability would be horrendous. The hip joint is encased in bone and gets alot of stability from that, this is the shoulders solution. The physio community goes through phases of if scapulohumoral rhythm is important to shoulder function/pain. Currently it is important, but it's not a great idea to have broad brush strokes. Treat the person infront of you and if the scap dysfunction is a driver then treat accordingly but if not move on.
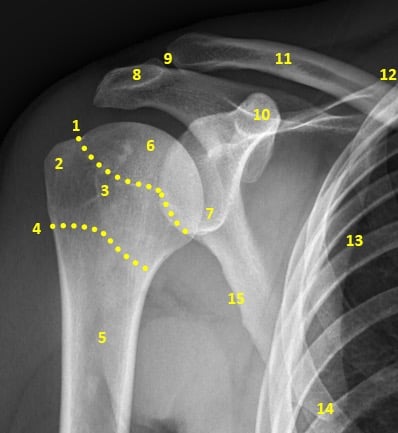
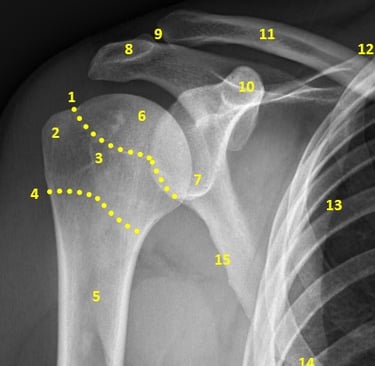
Structural Overview:
Joints
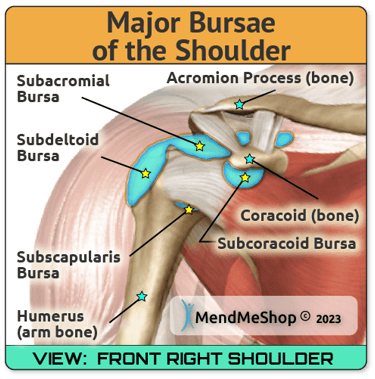
Bursae
In years past having bursitis was a diagnosis. It is not, it is a symptom of a larger mainly mechanical but sometimes traumatic problem. The bursae are there to decrease friction in areas of low tolerance. The problem is when they get aggravated they cause more friction and can be a secondary pain driver which leads to more disfunction.
The main two to be aware of are the sub deltoid and sub acromial bursa. Interestingly they can also be inflamed on imaging but the patient reports no major pain or dysfunction that could be related to the bursa.
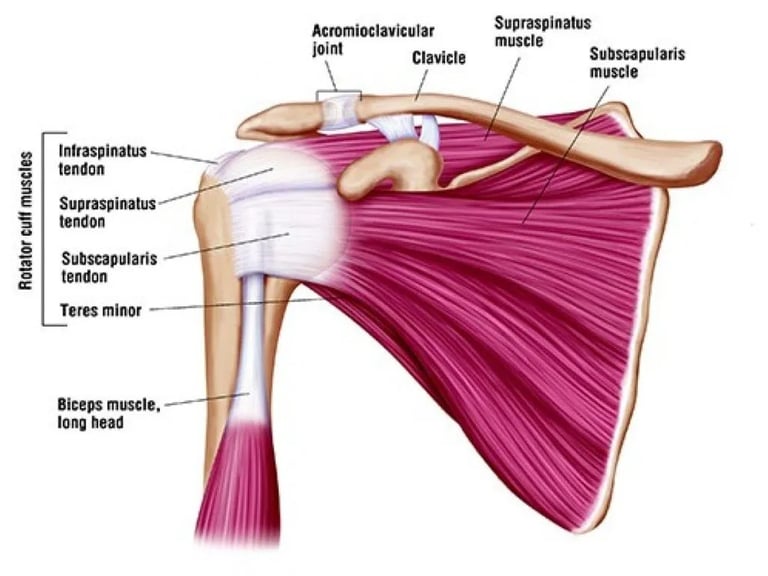
CUFF
Sadly the special tests taught at uni not only have poor diagnostic value but also are quiet off when it comes to testing what we think we are testing. The CUFF must work as a whole. This way it can help to centrate the humeral head in the glenoid and avoid unneeded rotationally forces. A. relaxed shoulder has rough 2cm of joint play in all directions. This shows how little the passive structures actually provide stability to the complex.
Supraspinatus: main action EXTERNAL ROTATION, does not INITIATE abduction
Infraspinatus: works best as a force couple with anterior shoulder and pecs. Cannot isolate with ER exercises.
Subscapularis: works best as force couple with post shoulder an upper back. Cannot isolate with IR exercises.
Teres Minor: works with other ADDUCTING muscle, adduction exercise poor use in rehab and does not assist in reducing impinging forces.
'Prime Movers'
We say prime moves loosely as there are no pure stabilising muscles and only moving muscles. The muscles around the shoulder can all work in a stabilising, moving, resisting and synergistic role as needed. The following is the most important function of the muscle at the shoulder, not all the actions it provides.
Deltoid: provides superior glide during abduction
Traps: Upper trap causes scapular upward rotation and cancels out depression. Lower trap causes upward rotation and cancels out elevation. Mid Trap: cancels out protraction.
Rhomboid: help to retract scapulae
Lats: could provide inferior glide abduction
Pecs: horizontally adduct humerus, assist in humeral adduction
Bicep: Provides anterior stability at the shoulder in neutral and throughout most actions.
Tricep
Serratus Anterior: Causes upward rotations and cancels out retraction.
Common Conditions
Dislocation: general described as a loss of congruency for a prolonged period. If the patient presents to the clinic with an obvious dislocation DO NOT attempt the reduce unless there are signs of neurovascular compromise. Generally patient will present after being discharged from the hospital and hopefully in a sling. If not a full sling is warranted. This allows time for the damaged passive structures to heal and stiffen up. Similar to an ankle sprain the shoulder can never be as stable as it once was post dislocation without a specific strength and conditioning program. Patient will often report that the joint was sitting out of place and required reduction at the hospital. Scanning may be required to rule out the presence of Bankart (ANTERIOR INFERIOR ASPECT or Hills-Sachs (SUPERIOR ASPECT) lesions. Basic Treatment: Sling (2 weeks generally), STR to avoid excessive muscle stiffness, scans, rebus the CUFF/shoulder girdle specific to patient needs.
Subluxation: generally less serious but if occurring often can indicate a more systemic issue such as hyper mobility or generalised shoulder instability. Sling is generally not indicated. Assess specific strength, endurance and stability this will guide the specific of rehab. Discuss patient around number of subluxations and any altered sensation during or post. Basic Treatment: KT tape, stability training in neutral then slowly moving to wide and wider ranges while maintaining good shoulder control.
SLAP Tear
Long Head of bicep Tendinopathy: This can be a diagnosis or just a symptom of a more general shoulder problem. Overhead athletes will generally get pure tendinopathy from a change in volume/technique, poor recovery and /or load. The reason why athletes GENERALLY get the diagnosis is that on testing of the shoulder the stability and strength is equal to the other side. For most people this is a symptom of some kind of shoulder dysfunction. The key is to determine if it is CUFF, shoulder girdle, scap movement or all three. While you treating the underlying problems still apply tendinpathy based rehab to the bicep. Basic Treatment: TPDN, taping, Isometrics in non painful positions, strength/endurance/stability for shoulder
Bicep Tenosynovitis
CUFF tear
CUFF tendinopathy
Traumatic Impingement: almost always caused by an impact with the arm overhead. Normally the patient would have been falling forward initially landing on the chest but rolling forward onto the arm pushing it into overpressure. It is important to clear of other concurrent injuries that could have occurred at the same time (ACJT, sublux, CUFF tear ect).
Shoulder Bursitis/Shoulder Impingement: in years past this was ok diagnosis but it focuses on the symptom and not the cause. Shoulder bursitis or Sub-acromial Bursitis (SAB) is generally an overload/overuse issue causes by poor shoulder mechanics. its up to you to decode the exact mechanical problem but generally it is due to a lack of SCAP upward rotation. Despite this patients continue to reach overhead asking more abduction from the humerus running into the bursa. Increase in fluid in the bursa can occur very rapidly or over the course of months. Patient over the age of 30 and smokers are typically more affected. Obviously those with hobbies and/or occupations overhead are also more prone. Basic Treatment: find the dysfunction, release overactive muscle (dry needling works very well, especially in lateral deltoid), rebuild under active muscles, start in neutral and slowly rebuild to front loading and overhead positions.
SCAP Dysfunction: in previous years how the scap moved was inconsequential. This can still be true for our geriatric patients post chronic CUFF tears and shoulder movement has compensated to a very functional level. For all our other patients it can play a huge factor or just part of the puzzle. Pain is often insidious and is away from the actual cause. treat the symptoms but focus on the cause. Look for asymmetry during the objective. Winging, excessive upward rotation, protracted resting position and see if these observations are worsened during isolated or functional tests. Pain during the pain arc can be present but not always. The above muscle function information will give you clues to what force couple may be dysfunctional. Basic Treatment: TPDN lateral delt, KT tape, self releases, specific rehab to address dysfunction.
CUFF repair
SC Joint dysfunction/First Rib
AC Joint Sprain: very common in contact sports, especially rugby union/league. Generally caused by FOOSH or direct contact to the shoulder. Patients will report very focused pain at the ACJt and have an increase in pain on AROM/PROM. It will be TOP and if severe enough unstable. Scarf test and resisted ACJt stress test are fairly reliable here and provide a good measure for isolated progression as pain decreases function increases. See the link for information on grades: https://www.physio-pedia.com/Acromioclavicular_Joint_Disorders . Basic Treatment: rigid tape to stabilise and pain relief, keep musculature firing in non-painful methods. As stability increases progress demand. Exit criteria needs to be based on demands of sport. A good rule of thumb for contact athletes is if they can perform a handstand wall walk with nil pain then they can at least return to training.
Shoulder Repair
Reverse Total Shoulder Replacement: often occurs after failed CUFF repair or traumatic accident. Much of the previous CUFF is sacrificed as the prosthetic joint is more similar to a hip joint and does not require the active stabilizers. Patient s often do very well. The protocol is there for a reason, FOLLOW IT. In addition, our role is to inspect for signs of infection, monitor for structural fails and guide the patient to the correct level of activity. Basic Treatment: protocol.
Frozen Shoulder: the latest research debates how much inflammation in the joint capsule is to blame. That being said this can be debilitating for those it affects. Much more common in females and often around menopause will it occur due to a mild injury, post surgery or gradually with no trigger. The cardinal signs see a loss of active and passive HBB, then ER and finally flexion/abduction. Timeframes can vary greatly but generally around the 18 month mark sees the full resolution of symptoms. Basic Treatment: maintain strength and range at shoulder/thoracic/elbow and wrist doing the different stages. Some practitioners are manipulating frozen shoulders 1/7 post CSI, the research is spotty currently.
Subjective Concepts
Although each subjective has many similarities you will find each body area has some key points to hit. This level of specificity at each joint ensures we do not miss obvious serious/sinister signs and gives us the right information to provide the right kind of treatment too.
Main Points:
-Traumatic vs chronic: general the groups tears/dislocations/fractures and tendon/bursa overload.
-Timeframe: Not just when the presentation started but also how long the pain lasts and how quickly it settles. This gives a great clue to the current level of tolerance to the structures.
-Loss of function: any loss of function could indicate a complete tear or subluxation. Worse case scenario stroke.
-Referral Pain/Pins and needles: If yes then this could indict the neck is at least partly involved or the main driver.
-Focal pain vs Widespread: Widespread pain that is not related to the neck could either mean multiple injury sites or active trigger points contributing.
-Bruising: This could be very benign such as a light impact and the bruising has no relation to the patient pain or dysfunction. Opposing this could indicate and extensive or multiple tears near the surface. Think pecs, lats, bicep.
-Painful actions (be specific): Each action involves different structures and in different ways. This can help in determining the diagnosis and as an objective test for progression. The painful arc as it relates to shoulder impingement can be useful but is not seen in every patient. HBB is very specific to joint capsule and long head of bicep tendon.
-Sports, work, hobbies: this gives you goals and can help guide your rehab in the mid to late stages. It also means we need to discuss if any modifications that may need to be made.
Objective Assessment
The order of the following can vary greatly depending on the presentation and injury stage of the patient. For example a patient in a chronic state and moderate pain levels should be taken through more functional tests if you think it will not aggravate to greatly. On the flip side if a patient comes in on crutches post ankle sprain observation, palpation and gentle special tests should be your mainstay.
Observation: muscle bulk, level of ACJT/collar bones, scars, discolouration, scap motion, passive thoracic position, HOH resting posture
Palpation: Feeling muscle bulk for levels of tone and asymmetry. Feel along boney land marks and joint lines (pain, asymmetry, joint space abnormalities).
Functional: Y excursion (for single arm stability and confidence), push up (scap stability and control, L vs R strength, compensations).
AROM: F/ABD/ER/HBB/SCAPTION. Look at scapular motions, shoulder hitching, comfort levels, compensations (forward HOH roll, neck working to stabilise).
PROM: Joint play F/AFT/INFERIOR (sulcus sign) for GHJt (done in sitting). Scap support to see effect of pain reduction or reduced tension. Flexion in supine, feel for SCJt roll and glide as shoulders moves.
'Special Tests'
Post Treatment
