A physiotherapy guide to whiplash
Dedicated to providing physiotherapists with the latest evidence-based practices for effective whiplash treatment and management, enhancing patient outcomes through objective testing and tailored treatment plans.
Whiplash Management for Physiotherapists
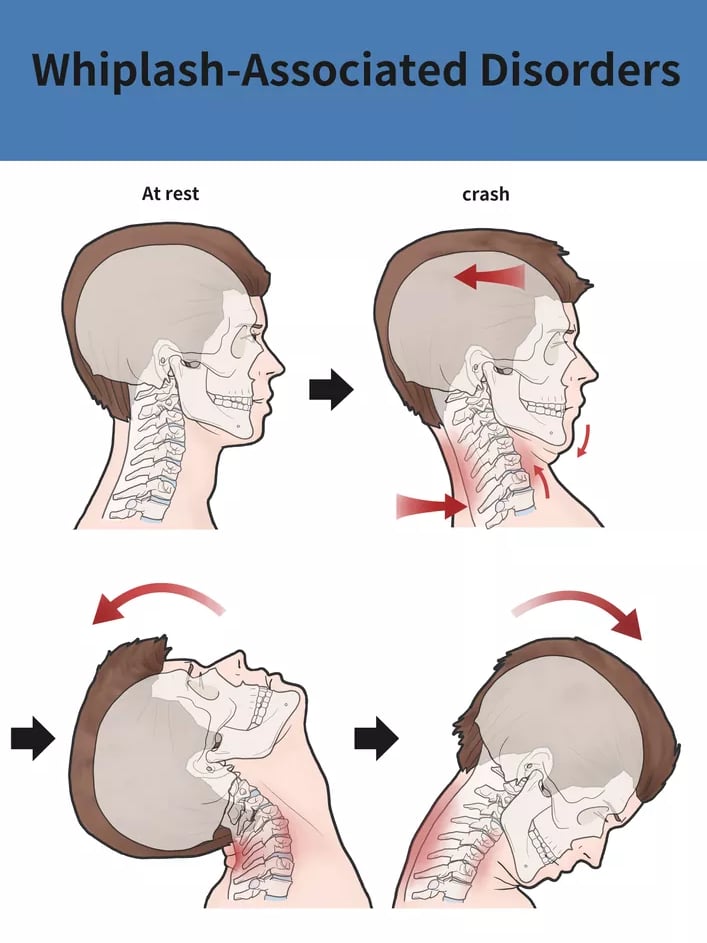
Whiplash is a common neck injury caused by a sudden forward and/or backward motion of the neck. It often occurs during motor vehicle collisions or high-impact sports, leading to pain, reduced range of motion, dizziness, and headaches. Below is an evidence-based guide for physiotherapists on recognizing, assessing, and managing whiplash-associated disorders (WAD).
Understanding Whiplash & Latest Evidence
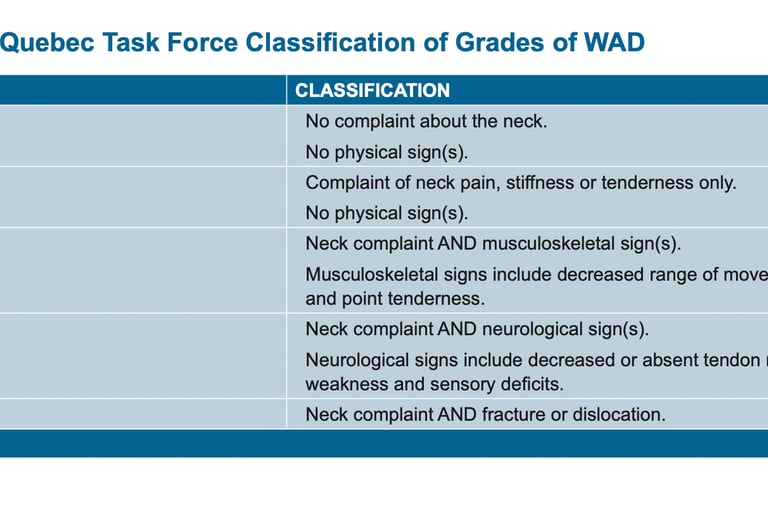
Whiplash-associated disorders are commonly categorized using the Quebec Task Force (QTF) classification system, which grades injuries from mild neck pain (Grade I) to neck complaints with neurological signs (Grade IV). Assess pain using the Visual Analogue Scale (VAS). Assess disability using the Neck Disability Index (NDI).
Early Mobilization: Encouraging gentle movement is generally more beneficial than prolonged immobilization, aiding in pain reduction and improved function.
Active Rehabilitation: Exercises focused on neck strength and endurance can minimize long-term disability.
Psychological Factors: Chronic whiplash often involves psychological and social components; addressing these early can positively impact outcomes.
Education: Providing reassurance about a typically favorable prognosis can help patients return to normal activities sooner.
Objective Testing
A comprehensive evaluation is essential for accurately characterizing whiplash severity and guiding treatment decisions. Common objective measures include:
Range of Motion (ROM) Testing: Use a goniometer or inclinometer to measure cervical flexion, extension, lateral flexion, and rotation.
Strength & Endurance Tests: Conduct manual muscle testing and endurance assessments (e.g., cranio-cervical flexion test) to gauge neck flexor and extensor capabilities.
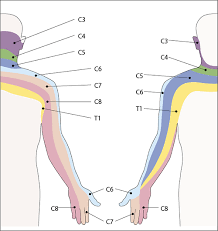
Neurological Examination: Look for sensory deficits, altered reflexes, or muscle weakness, as these can indicate nerve root involvement.
Functional Scales: Instruments such as the QTF, Neck Disability Index (NDI) or Visual Analog Scale (VAS) quantify functional limitations and track improvements over time.
Postural Assessment: Observe both static and dynamic posture, noting any compensatory patterns.
Proprioceptive changes: JPE, balance and posture, sensorimotor patterning (can they catch a ball whilst maintaining body stability.
Treatment Plans
Comprehensive treatment for whiplash typically involves a blend of manual therapy, exercises, and patient education:
Manual Therapy
Soft tissue mobilization to reduce muscle tension and boost circulation.
Joint mobilizations or manipulations (if clinically indicated) to restore normal cervical mechanics.
Therapeutic Exercises
Deep cervical flexor strengthening (e.g., cranio-cervical flexion exercises).
Scapular stabilization to support neck function.
Progressive resistance exercises for the neck and upper back.
Progressive Activity & Conditioning
Incremental return to daily tasks, guided by pain tolerance and functional capacity.
Low-impact cardiovascular work (e.g., stationary biking) to enhance overall fitness.
Patient Education & Self-Management
Reassurance that most whiplash cases have a favorable prognosis with active rehab.
Ergonomic advice for workplace and daily habits.
Home exercise programs for consistent progress between sessions.
Pain Management Techniques
Modalities (heat, cold, TENS) for short-term pain relief if appropriate.
Relaxation and mindfulness practices to address stress-related muscle tension.
Proprioceptive Changes in Whiplash
Research indicates that whiplash-associated disorders can disrupt the normal sensorimotor control of the cervical spine. This often includes altered joint position sense, impaired balance, and diminished postural stability. According to Kristjansson and Treleaven (2009), such proprioceptive dysfunction is linked to ongoing neck pain, dizziness, and an increased risk of chronic symptoms. These changes can be attributed to:
Muscle Spindle Disturbance: Rapid hyperextension or hyperflexion of the neck may damage or overstretch muscle spindles, reducing their ability to accurately detect changes in muscle length.
Altered Neuromuscular Control: Inflammatory mediators, pain, and protective muscle guarding can impede the normal neurological feedback loops necessary for accurate proprioceptive input.
Joint Capsule/Mechanoreceptor Injury: High-impact forces can affect ligamentous and capsular structures in the cervical spine, further impairing mechanoreceptor function.
References: Kristjansson, E., & Treleaven, J. (2009). Sensorimotor function and dizziness in neck pain: Implications for assessment and management. Journal of Orthopaedic & Sports Physical Therapy, 39(5), 364-377. Treleaven, J. (2017). Dizziness, unsteadiness, visual disturbances, and sensorimotor control in neck disorders. In: Jull, G., Moore, A., Falla, D., Lewis, J., McCarthy, C., & Sterling, M. (Eds.), Grieve's Modern Musculoskeletal Physiotherapy (4th ed.). Elsevier.
Exercises to Address Proprioceptive Deficits
Rehabilitation programs that specifically target sensorimotor control have been shown to improve joint position sense and reduce neck pain. Below are recommended exercises:
Cervical Joint Position Error (JPE) Training
Use a laser pointer or head-mounted device that projects a beam onto a target (e.g., a wall grid).
Ask the patient to rotate or flex/extend the neck and then return to the neutral position, aiming to align the beam with the initial starting point.
Perform multiple repetitions, gradually increasing complexity (e.g., eyes closed, varied speeds).
Oculomotor Control Drills
Practice eye-following exercises with a stationary or moving target to enhance coordination of eye and head movements.
Incorporate smooth pursuit and gaze stabilization exercises (turning head side-to-side while maintaining stable fixation on a single point).
Balance and Postural Stability Exercises
Introduce single-leg balance tasks, progressing to unstable surfaces (e.g., foam pads or balance boards).
Combine balance challenges with head movements (looking up/down or side-to-side) to replicate functional scenarios.
Sensorimotor Integration
Include dynamic tasks such as reaching and catching a ball while maintaining cervical stability.
Perform multi-plane movements (lateral flexion, rotation) with added visual or auditory cues to reinforce sensorimotor retraining.
Scapular and Core Stabilization
Reinforce proximal stability to reduce excessive compensatory motions that might hamper accurate cervical proprioception.
Exercises like prone I/Y/T or seated rows can enhance scapular control, indirectly supporting neck posture.
References: Jull, G., Falla, D., Treleaven, J., Hodges, P., & Vicenzino, B. (2009). Retraining cervical joint position sense: The effect of two exercise regimes. Journal of Orthopaedic & Sports Physical Therapy, 39(5), 330-338. Sterling, M., Jull, G., Vicenzino, B., & Kenardy, J. (2003). The development of motor system dysfunction following whiplash injury. Pain, 103(1-2), 65-73.
Prognosis & Follow-Up
Most individuals show notable improvement within weeks when treated proactively. Persistent symptoms beyond six weeks may require a specialized or multidisciplinary approach, potentially incorporating cognitive-behavioral therapy and more intensive rehabilitation. Regular re-assessment ensures the treatment plan remains aligned with patient progress and goals.


Case Study: Whiplash-Associated Disorder (WAD)
Patient Profile
Name: Sarah M. (fictional)
Age: 32
Occupation: Office worker
Activity Level: Moderately active (gym 2-3x per week, occasional running)
Primary Complaint: Neck pain and headaches following a car accident
History of Presenting Condition
Sarah was involved in a rear-end motor vehicle accident two weeks ago. She experienced immediate neck stiffness, pain, and a mild headache after the incident. She went to the emergency department, where imaging ruled out fractures or serious injury. She was advised to rest and take pain relief.
Since the accident, her symptoms have worsened. She reports:
Neck pain (4-7/10) that worsens with prolonged sitting or turning her head.
Headaches (pressure-type, occipital and temporal).
Limited cervical range of motion, particularly in rotation and lateral flexion.
Intermittent dizziness when moving quickly or standing up.
Increased shoulder tension and a mild sensation of tingling in her right hand.
Assessment Findings
Subjective Assessment:
Pain location: Cervical spine (C2-C6), upper trapezius, occiput.
Pain behavior: Worse with prolonged sitting, driving, and looking down at a screen. Improves slightly with movement but flares up unpredictably.
Sleep disturbances: Reports difficulty finding a comfortable position at night due to neck pain.
Functional limitations: Difficulty focusing at work, avoiding gym sessions due to fear of making it worse.
Objective Assessment:
Posture: Forward head posture, mild thoracic kyphosis, increased upper trapezius tone.
Cervical ROM:
Flexion & extension: Reduced, pain at end range.
Rotation: Limited bilaterally (R > L).
Lateral flexion: Painful and restricted.
Palpation:
Hypertonicity and tenderness in upper trapezius, SCM, levator scapulae.
Cervical facet joint tenderness (C2-C6).
Neuro Exam: No red flags, mild right C6 dermatome hypersensitivity.
Special Tests:
Spurling’s Test: Negative.
Cervical Joint Position Error Test: Mild deficit in proprioception.
Smooth Pursuit & VOR Testing: Slight dizziness with quick head movements.
Neck Flexor Endurance Test: Reduced endurance (5 sec hold vs. normal ~30 sec).
Diagnosis & Classification
Whiplash-Associated Disorder (WAD) Grade II (based on Quebec Task Force classification):
Soft tissue involvement (muscle guarding, pain, joint stiffness).
Sensorimotor dysfunction (proprioceptive impairment, dizziness).
No neurological deficits (i.e., no weakness, reflex changes, or red flag symptoms).
Please answer these questions and email them to me :) - we can go over them in mentoring this week - remember no need to be perfect - just imagine it was a real patient :)
Manual Therapy Approach
Early Stage (Week 1-2): What manual therapy techniques would you use to reduce pain and improve mobility while avoiding excessive guarding?
Progression (Week 3-6): How would you transition from passive treatments to active movement strategies, and what techniques would you prioritize?
Exercise Approach
Early Stage (Week 1-2): What key exercises would you prescribe to activate neck musculature and improve mobility without aggravating symptoms?
Progression (Week 3-6): How would you progress strengthening and proprioceptive training while ensuring a safe return to functional activities?
Education Approach
Patient Reassurance: What key messages would you give the patient early on to reduce fear-avoidance and encourage movement?
Self-Management: What strategies and long-term prevention tips would you provide to help the patient manage symptoms independently?
Whiplash Management Guide
Latest evidence and treatment plans for physiotherapists to effectively manage whiplash injuries.
